34 year old male with vomiting,hiccups and cough
Not a known case of Dm,Tb, epilepsy, asthma,HTN
Personal History
Diet- mixed
Appetite- decreased
Bowel and bladder- regular
Sleep- regular
Addictions-alcoholic(16 yrs back he started drinking),chews betel(starting he used to take 1 packet and now he is taking 10 packets daily)
FAMILY HISTORY:
His father died due to hernia
His mother died due to kidney failure
General examination:
Patient is conscious coherent cooperative well oriented to time place and person moderately built and nourished
Vitals:
Temperature- afebrile
RR-16cpm
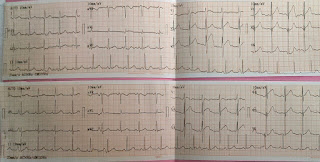
PR 75bpm
BP 130/70 mm hg
Pallor,icterus, cyanosis,generalized lymphadenopathy,edema - absent
SYSTEMIC EXAMINATION:
Abdomen flat
No distension
No engorged veins
No visible pulsations
No scars
Palpation-
All inspectory findings are confirmed in Palpation
No tenderness
No guarding rigidity
No Hepatomegaly
No splenomegaly
Percussion- normal
Auscultation-
Bowel sounds are heard
1. IVF- 0.9 NS @ 100 ml/hrRL- @ 100 ml/hr2. Inj. Thiamine 200 mg in 100 ml NS IV/TID3. Inj. Zofer 4 mg/ IV/ TID4. Inj. Metoclopramide 10 mg/IV/SOS5. Syp. Lactulose 30 ml/ PO/ HS6. Tab. Udiliv 300 mg PO/BD
7. Inj. Vit K 20 mg IV/STAT (100 ml NS) followed by Inj. Vit K 10 mg in 100 ml NS/IV/BD8. Syp. Mucaine gel 15 ml/PO/TID9. Tab. PAN-D (40/30) PO/OD10. Watch for any bleeding manifestations11. Watch for signs of Hepatic encephalopathy12. Strict I/O charting13. Monitor vitals BP, PR, Temp14. Inform SOS
7. Inj. Vit K 20 mg IV/STAT (100 ml NS) followed by Inj. Vit K 10 mg in 100 ml NS/IV/BD






























Comments
Post a Comment